The irrational use of medicines, a major driver of antimicrobial resistance (AMR), is often perpetuated by those who should be best able to stop it—health care professionals such as doctors and pharmacists. This, of course, raises an important question: why do health care professionals continue to practice potentially harmful behaviors? In many cases, the answer is quite simply that they’ve never learned not to.
Ensuring that pre-service education for health services professionals including training on issues related to AMR and rational medicine use (RMU) is therefore an important step toward improving rational use practices in the health care facilities and communities those professionals will serve in future. Appropriate pre-service curriculum reform and training is a cost-effective intervention that has the potential to strengthen health systems. However, traditional health services curriculums give little attention to practical topics relating to AMR and RMU. SIAPS is endeavoring to address this gap by integrating these subjects into university curriculums, ensuring that students view these issues as important to public health—and, therefore, important to their future careers.
SIAPS and its predecessors have helped to design and launch several programs aimed at training health services professionals in the areas of AMR and RMU. Based on these experiences, SIAPS has published a guidance document on revising pre-service curriculum to incorporate RMU topics. The document outlines and describes steps in reforming curriculum to integrate RMU, AMR and pharmacovigilance topics and provides several tools, templates and examples. Two examples of such curriculum redesign are outlined below.
Namibia: Integrating RMU and AMR into the UNAM School of Pharmacy Curriculum
SIAPS and its predecessor have assisted in the development and academic activities of the University of Namibia (UNAM) School of Pharmacy, the first pharmacy training program in the country. With an eye to keeping the country’s pharmacists focused on public health issues like AMR from the start, SIAPS also helped to consolidate the school’s curriculum, emphasizing pre-service training on RMU and AMR for undergraduate pharmacy students.
While UNAM’s undergraduate pharmacy curriculum included several topics on RMU in its prospectus and pharmacy practice study guide, it was lacking detailed information on the implementation of those topics. To fill this gap, SIAPS supported UNAM in developing a customized course on RMU, designing a curriculum implementation framework, instructional delivery design, and course materials, including detailed instructors’ guides.
The detailed RMU implementation design, which emphasizes case-based and self-directed learning methodologies, was first offered in August 2014. SIAPS continues to provide follow-up support to build UNAM’s capacity to monitor and evaluate the effectiveness of the course, refine the course materials, document and publish results and lessons learned, and apply this approach to additional topics within the pharmacy program and with additional academic disciplines at the university.
Zambia: Filling in the Curriculum Gaps at UNZA School of Medicine
The Rational Pharmaceutical Management (RPM) Plus and Strengthening Pharmaceutical Services (SPS) programs, both predecessors to SIAPS, helped the University of Zambia (UNZA) School of Medicine implement AMR and RMU components into its medical school curriculum.
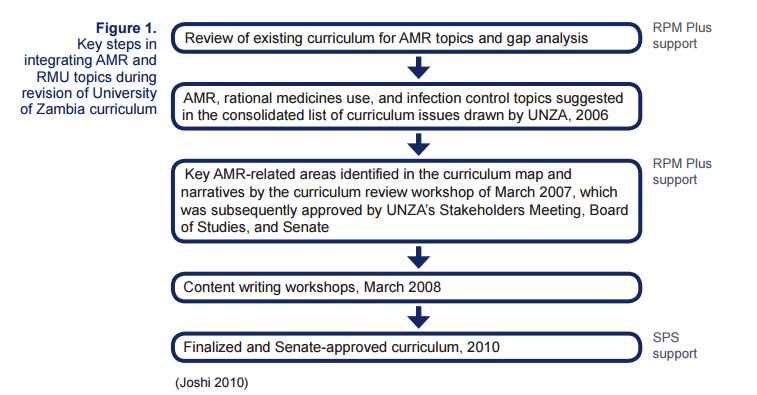
RPM Plus first helped the university perform a review of its existing curriculum, identifying gaps in AMR/RMU education. It was determined that exposure of medical students to AMR/RMU topics was inadequate on many levels: there were no specific course modules dedicated to AMR, only passing discussion of serious AMR threats such as methicillin-resistant Staphylococcus aureus, and students were not given any specific education related to issues of patients’ misconceptions about antimicrobial treatment, self-medication, or poor adherence to treatment regimens.
RPM Plus and its successor SPS then helped to incorporate topics of public health importance relating to AMR and RMU into the revised medical school curriculum. The revised curriculum was approved by the Zambian Senate in 2010, and thereafter used at the university.
Authors: Mohan P. Joshi, Principal Technical Advisor and Cluster Lead for Pharmaceutical Services, and Elyse Franko-Filipasic, Senior Communications Associate

