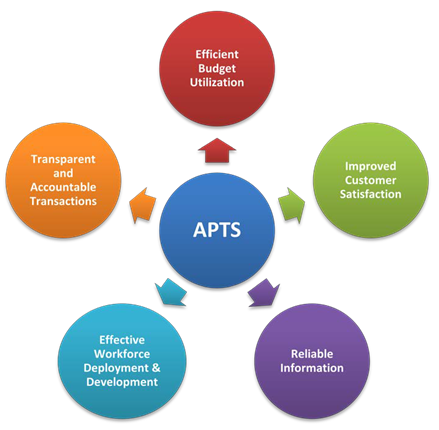
Ethiopia’s pharmaceutical system suffers from major structural and systemic problems around transparency and accountability; recording/ documentation/ information management, human resources, workflow, and quality of services. The US Agency for International Development (USAID)-funded Systems for Improved Access to Pharmaceuticals and Services (SIAPS) is scaling up the use of a leading-edge systems tool that introduces transparent and accountable pharmaceutical transactions and services. Auditable Pharmacy Transactions and Services (APTS) introduces transparent and accountable pharmaceutical transactions and services that result in a continuous supply of essential medicines, optimal budget utilization, and improved pharmacy services.
Challenges in Ethiopia’s Pharmaceutical Service System
Access to essential medicines and their rational use have long been a challenge in Ethiopia. The following is a summary of the major structural and systemic problems that have obstructed the effective management of the country’s pharmaceutical system.
Accountability and transparency: The procurement and dispensing of pharmaceuticals do not follow a standard and transparent system capable of providing the necessary information relevant for effective monitoring and auditing. The results are frequent stock-outs, expiry, theft, and pilferage of medicines, with no one held accountable.
Legal instruments and enforcement: The management of medicines and provision of pharmaceutical services at health facilities has not been adequately covered by relevant legislation or regulation. There is no enforcement of the laws/regulations that do exist to protect the safety of clients, ensure proper utilization of resources, and deter professional malpractices.
Systems and Tools: The pharmaceutical transactions and services taking place at health facilities are not supported by well-designed and up-to-date systems and documentation. The system in place has not been adequate enough to track consumption, inventory discrepancies, wastages, product overstock or under-stock.
Efficiency in utilizing limited budget: The selection and prioritization of medicines has not been guided by accepted procedures so as to ensure availability of essential to majority of the population.
Protection from financial and other risks: There is no mechanism to protect pharmacy personnel and other health facility workers, such as store keepers, dispensers and cashiers, against financial and legal liabilities.
Infrastructure and equipment/facilities: The pharmacy unit in health facilities rarely is provided with adequate and secure space. There is no suitable area for dispensing medicines and counseling patients. There is no waiting area for patients or offices for pharmacists. There is no separate area for extemporaneous preparation of medicines. Drug information services are seldom in place. In addition, essential equipment including refrigerators, shelves, lockable cabinets, tablet counting trays, medicine envelopes, and labeling stickers are not supplied to meet existing demands. In most cases, pharmacies at health facilities do not have easy access to transport to make timely procurements of medicines from suppliers.
Human resource development and deployment: The allocation, training, performance evaluation and retention of human resource for pharmacy services have not been adequately addressed. The number and professional mix of pharmacy staff (pharmacist, druggist, accountants, cashiers, data clerks, porters, cleaners, and guards) do not follow standards or guidelines. There is no mechanism to measure the level of effort of dispensing pharmacists and the result of their work is not measured.
Organization and management: The way in which the pharmacy unit is organized within the health facility does not enable the unit to respond to the current needs of patients for pharmacy services and creates inconvenience to clients.
Work Flow: The process of dispensing of medicines is laborious and time-consuming due to a disorganized workflow, thereby inconveniencing clients.
Forging Successful Partnerships
Responding to the difficult challenges of its broken pharmaceutical management system, Ethiopia’s Ministry of Health (MoH) introduced the Hospital Reform Implementation Guidelines (EHRIG). The USAID-funded Strengthening Pharmaceuticals Systems (SPS), the predecessor program to SIAPS, developed the EHRIG chapter on pharmaceutical services. USAID/SPS assisted the MoH in preparing the 12 standards of essential pharmacy services for hospitals.
The next step in USAID/SPS support to the MoH was to develop implementation guidelines and then pilot the operationalization at Debre Markos Hospital. Today, USAID/SIAPS is scaling up the use of APTS in other regions—including the Amhara, Tigray, Addis Ababa and the Southern Nations and Nationalities Peoples Region. Currently, APTS is being implemented at ten hospitals and one Health Center. The Government of Ethiopia is in the process of institutionalizing use of the model through appropriate legislation.
USAID/SIAPS, and its predecessor project USAID/SPS, forged a successful partnership with the Government of Ethiopia and other stakeholders throughout the country to achieve results. USAID/SIAPS not only worked with the Ministry of Health at the federal level, but with the Regional Health Bureaus and the Regional Finance and Audit Bureaus as well.
APTS: Innovation in Pharmaceutical Management
The Auditable Pharmacy Transactions and Services (APTS) is a package of interventions that produces transparent and accountable pharmaceutical transactions and services.
Developed in 2012, this package of interventions includes the following:
- Revise receiving and issuing vouchers at pharmacy stores in health facilities to make them appropriate for pharmaceuticals
- Create medicines sales tickets and related financial tools
- Put in place medicines dispensing registers for credit sales
- Generate daily and monthly reporting forms both for transactions and services
- Train pharmacy and accounting staff, including cashiers and auditors, to implement APTS
- Develop and disseminate manuals and forms for APTS implementation
- Take initial inventory of all medicines and supplies at the health facility as a baseline for subsequent inventory taking and auditing
- Strengthen drug and therapeutic communities (DTCs) to develop or revise hospital specific medicines list
- Support DTCs to prioritize the facility specific medicines list VEN followed by reconciliation with ABC values
- Conduct regular stock status/stock turnover analysis and present results to DTCs for decisions on subsequent actions on procurement, stock transfer, and prescribing
“APTS is a prime example of a best practice in strengthening health systems. APTS responded to a critical need, was developed and operationalized as a collaborative effort with stakeholders, and is now owned by the Government of Ethiopia.”
The Result: Improved Governance and Better Service Delivery
The preliminary results from Debre Markos Hospital show improvements in governance and pharmaceutical service delivery. The following are some of the results.
- There is a hospital specific medicine list in use that

Pharmacy accountant compiling daily summary in APTS takes into account the disease pattern and health needs of the catchment population
- The implementation of an ABC value analysis and identifying medicine use problems has made the procurement and use of medicines evidence-based
- The percent of medicines procured according to the hospital-specific medicines list increased from 35.4% to 97.5%
- A continuous physical inventory of products both at the store and dispensary is made possible
- Financial resources available for medicines procurement increased by 89.1% between June 2010/11 and June 2011/12 due to the high turnover of medicines and the substantial retention of income from medicines sales
- Internal and external audit reports indicate that wastage of medicines due to misuse, theft, and pilferage has significantly decreased
- Expiry of medicines was reduced dramatically. Since December 2011, expiry of medicines has consistently been below 2%, the most recent figure being 0.5%
- The availability of indicator medicines has increased over time to 100%.
- A robust system that ensures transparent and accountable transactions is in place, enabling effective auditing
- Outpatient pharmacies were reorganized resulting in improved work flow and dispensing counseling services.
- Improved patient satisfaction with services provided which has increased from 33% in 2010 to 85% in 2012.
- Initiation of pharmaceutical care services for patients with chronic illnesses in a separate private counseling and dispensing room resulted in improved documentation and adherence to treatment.